Provider Credentialing Services in Alaska Just $59
Provider Credentialing services @dollar 59
- Cost reduction by 50%
- Guaranteed quality work
- Weekly analysis & monthly reporting
- Effective references
CONTACT US
7 key steps of Credentialing Process in Alaska
- Identify the Required Documents
- Prioritize Insurance Companies
- Check for Accurate Information
- Completing the CAQH
- Wait for Verification
- Following Up
- Recertification
Medical Billing & Coding Hub-Best Credentialing Services in Alaska For Private Practices/Solo Providers/New Setup/ New Practice
We are the Top rated professional Medical billing company working in Alaska to ensure an effective workflow with end-to-end Revenue Cycle Management which fulfil the needs of the Provider due to our technology base trusted solutions.
Medical Billing & Coding Hub Medical Billing Company offer over 40 Medical Billing Specialties to all Physicians/solo Provider/Practice owner. The proven track record of efficient billing solutions which lead to timely reimbursements make us one of the #1 Medical Billing Company in USA. From independent practices to hospitals, we offer customized billing solutions
Medical Practices Who Can Use Our Services
- Medical practices of all sizes
- Solo Physicians
- Independent Medical Practice Groups
- Medical Clinics
- Non-Emergency Medical Transportation (NEMT)
- Physician Groups
- Hospital-owned Physician Practices and Groups
- Urgent Cares
- In-home health services providers
- Laboratories
- Freestanding Emergency Centers
- Hospitals
Our Expertise









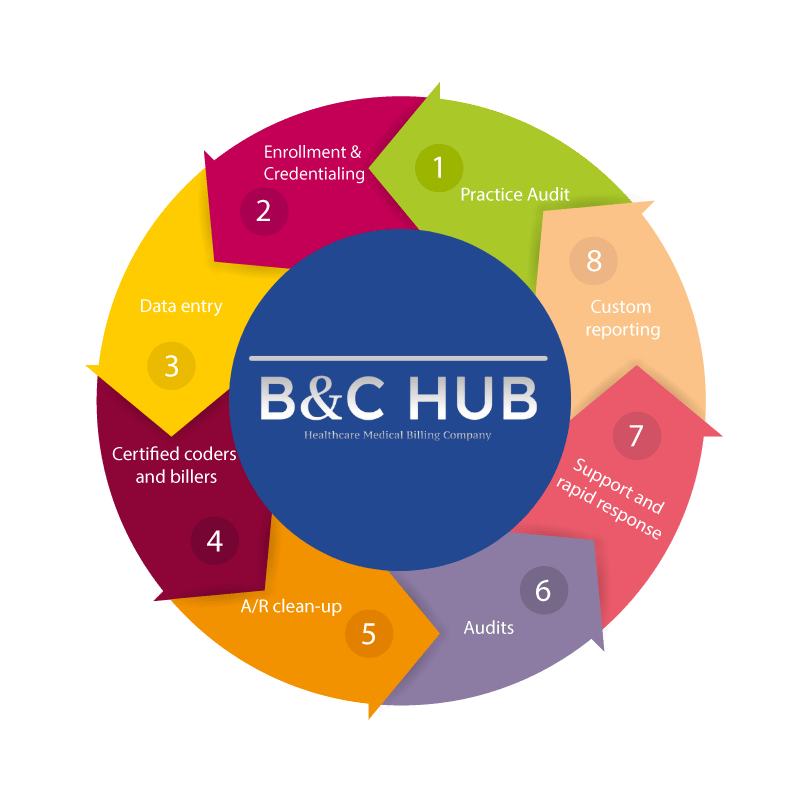
Physican Credentialing Process in Alaska
Primary Source Verification: Medical Billing & Coding Hub is among the top accredited physician credentialing companies that perform a primary source verification for the individual medical in-network provider to verify whether he acquired a valid license, certification, or registration to practice a profession as it is a primary requirement of health insurance companies.
Document Verification: Medical Billing & Coding Hub document verification process involves the next level of accuracy verification after the primary source verification, where the programs like Modio and Ready Doc are utilized to automate the credentialing process, including cross-referencing resume and application information with AMA profiles, medical schools, the OIG, and more..
Data entry :Although the digital revolution has accelerated the use of electronic medical records the complexities regarding medical data entry require healthcare providers to acquire data entry services. In this context, Medical Billing & Coding Hub is always available to take a look at your patient’s records that are needed to enter, organized, maintained, archive, and retrieved whether you are an entire hospital, outpatient facility, multi or a solo practitioner. Based on the scope of your requirements our concerned workforce utilizes innovative technologies to deliver you the best output.
Data Scrubbing: After successfully submitting our initial application, payers verify our healthcare providers’ documentation, i.e., Active License, DEA, PLI, NPI, Taxonomy, etc. If all documents are up to date and additional information is not required, apps are sent to the next enrollment phase.
Credentialing: Once the Data Scrubbing is completed through online portals (i.e., CAQH, Availity, PECOS, Optum, ePaces, etc.) or Mailed/Faxed documents, the provider/group can successfully be credentialed in the insurance system/directory.
Enrollment & participation:After getting credentialed with the payer, they proceed with our enrollment request to consider our provider/group as an In-Network or Participating Provider. Upon acceptance of this enrollment application, payers send us a formal contract & fee schedule to sign; in this way, our provider becomes a contracting & PAR provider.
Re-certification:Medical Billing & Coding Hub provides re-credentialing additionally in its medical credentialing services, ensuring the credentials provided by the medical practitioner are accurate and reviewing them regularly for additional verification.
Outsource Credentialing Services to Medical Billing & Coding Hub Services
Our physician credentialing experts have developed and maintained strong relationships with third party payers to allow for quick contract resolution. Our persistent tenacity ensures that you application is processed within a reasonable amount of time. We take all the paperwork and hassle out of your hands!
Most importantly, do not assume that all of these carriers and/or networks are going “back date” your participation. Most DO NOT! Call Outsource Management Group and we will assist you with your planning. We have discount price packaging available
Medical Billing & Coding Hub Healthcare Services promises to offer the best credentialing services, focusing on almost every medical billing or patient cycle aspect. We work to ensure the most available timely compensation for our patients. The quicker the invoice can be prepared, the faster and simpler the compensation is provided. With this in mind, we're running 24x7, and we've committed billers and billing experts to work while you sleep.

Medical Billing & Coding Hub customer can get
Up to
Reduce your administrative burden with our experts
Well trained and always stays updated about the recent changes in the Cardiology specialty.
Successful in processing medical claims with both commercial insurance companies and federal payers like Medicaid and Medicare.
Expert in eliminating any risk of losses, reducing costs and helping you achieve improved clinical & operational efficiency.

Benefits of Choosing Medical Billing & Coding Hub:
- FREE RE-CREDENTIALING SERVICES (ALL CLIENTS)
- FREE CREDENTIALING SERVICES (ONLY BILLING CLIENTS)
- FREE CODING SERVICES (ONLY BILLING CLIENTS)
- FREE ERA,EFT,EDI SERVICES (ALL CLIENTS)
- FREE EHR. SERVICES
- FREE 30 DAYS TRIAL BASE PRACTICE AUDIT
By Outsourcing you can get 700% cost effective
Credentialing Companies vs Medical Billing & Coding Hub
| Brackets of Collections | Other Companies | Outsource to Medical Billing & Coding Hub |
|---|---|---|
| Credentialing Services( Federal payers) Each Payer | 300$ | 59$ |
| Commercial Payer | 200$ | 59$ |
| EFT setup | 100$ | No Charges |
| ERA | 100$ | No Charges |
| Portal setup/availity | 100$ | No Charges |
| Re Credentialing | 100$ | No Charges |
GET YOUR FREE REVENUE CYCLE MANAGEMENT ASSESSMENT
Evaluate your Practice Performance
We offers free revenue cycle assessments (RCAs) to help large and small practices to work smarter, not harder. Are you performing to your full potential?
Frequently Asked Questions

Credentialing is the process of verifying and evaluating a healthcare provider’s qualifications, education, training, and experience to ensure they meet the standards and requirements of a healthcare organization or insurance payer.
Credentialing helps ensure that healthcare providers are competent and qualified to provide safe and effective care to patients.
All healthcare providers, including physicians, nurse practitioners, physician assistants, and other allied health professionals, need to be credentialed.
California healthcare providers must meet the credentialing requirements of the California Medical Association (CMA) and the California Department of Insurance (CDI).
The CPA is a standardized application used by healthcare providers to apply for credentialing and privileging in California hospitals and health systems.
The CMB is responsible for licensing and regulating physicians and surgeons in California. The CMB verifies the credentials of physicians and surgeons as part of the licensure process.
Healthcare providers must enroll with the Centers for Medicare and Medicaid Services (CMS) and meet the credentialing requirements of the Medicare Administrative Contractor (MAC) for California.
Healthcare providers must enroll with the California Department of Health Care Services (DHCS) and meet the credentialing requirements of the Medi-Cal program.
Healthcare providers must meet the credentialing requirements of each commercial insurance payer, which may vary.
The credentialing process can take several weeks to several months, depending on the complexity of the application and the speed of the credentialing process.
Healthcare providers typically need to provide documentation of their education, training, licensure, certification, and malpractice insurance, as well as other relevant credentials.
Credentialing is typically required when a healthcare provider joins a new healthcare organization or insurance payer, or when their credentials need to be updated or reverified.
