Medical Billing and Audit Services
Enjoy effortless and error-free Medical Billing and Audit services and the newest billing systems to increase claims acceptance rate, maximize revenue and receive prompt reimbursements.
- Cost reduction by 50%
- Guaranteed quality work
- Weekly analysis & monthly reporting
- Effective references
CONTACT US
Revenue Cycle management Audit Process- Trusted healthcare experts
- Identify the issues
- Obtain or define standards
- Collect data
- Compare performance with standards
- Implement change
- Re-audit
Medical Billing and Coding Hub-Best Medical Billing Audit Services For Private Practices/Solo Providers/New Setup/ New Practice
We are rated the highest Medical Billing Company in California with professional Services and an advanced workflow for 40+ Specialties and audit Revenue Cycle Management that is provider focused while achievable with our trusted solutions per technology base.
At Medical Billing Company, we strive to achieve efficiency in the auditing process rest assured that you will be among the first people paid. This has made us the number one Medical Billing Solution Provider as we cater for all types of practices from individual practitioners to large hospitals.
Medical Practices Who Can Use Our Audit Services
- Medical practices of all sizes
- Solo Physicians
- Independent Medical Practice Groups
- Medical Clinics
- Non-Emergency Medical Transportation (NEMT)
- Physician Groups
- Hospital-owned Physician Practices and Groups
- Urgent Cares
- In-home health services providers
- Laboratories
- Freestanding Emergency Centers
- Hospitals
Our Expertise
Medical Billing and Coding Hub specializes in comprehensive Medical Billing Audit Services, ensuring accuracy and compliance. Our expertise in Revenue Cycle Management streamlines processes, maximizes reimbursements, and improves financial performance for healthcare providers.









Our Medical Billing Audit Services
Our company Medical Billing and Coding Hub provides a range of offerings, such as Invoicing, Medical Credentialing Services and Patient Assistance.
Practice Audit
Practice overall performance for decision making process.
Credentialing
Fast and easy in-network enrollment with PPO, HMO, DMO and Medicaid.
Coding
This will allow for coding accuracy, clinical documentation, compliance and insurance contractual agreements.
Billing
Collect what you're rightfully owed from insurance companies.
Insurance Verification
Less denials and more reimbursements at incredibly affordable prices.
Hippa compliance
Friendly and effective strategies and best practices to get outstanding patient balances paid.
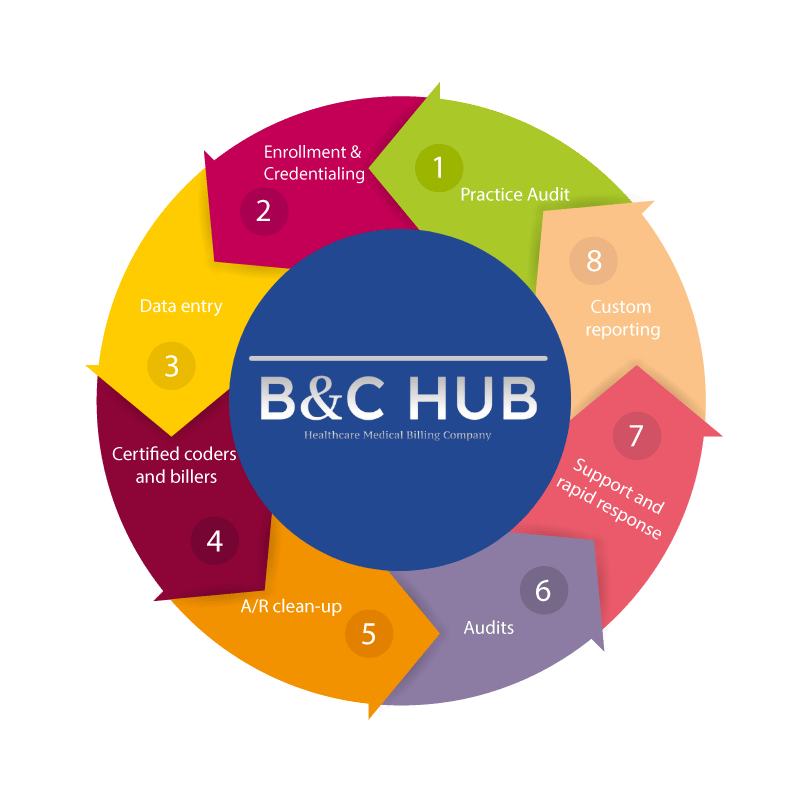
Our Medical Billing Process- Audit compliance
Methodology Planning: In the first stage, our auditors conduct internal or external reviews of medical records for coding accuracy, policies, and procedures to ensure an organization runs efficiently.
Develop Effective Audit Strategy: After the medical claims review, our auditor will determine whether we will use a prospective or retrospective strategy. This strategy helps identify and correct problems before sending claims to the insurance company.
Examine Records In EHR: At this stage of our company's standard process, our auditors check billing reports, charges, codes, and other censorious records to maximize cash flow and reduce claim denials. We follow the following recommendations at this stage.
Rectifying audit Contest: In the regulatory compliance practice revenue cycle management process, If the detailed report identifies any issue that could result in errors and claim denials, our company auditors identify areas to correct them within the shortest period.
Streamline Your Practice -Maximum Reimbursement
Medical Billing and Coding Hub specializes in comprehensive Medical Billing Audit Services, ensuring accuracy and compliance. Our expertise in Revenue Cycle Management streamlines processes, maximizes reimbursements, and improves financial performance for healthcare providers. Medical Billing and Coding Hub specializes in comprehensive Medical Billing Audit Services, ensuring accuracy and compliance. Our expertise in Revenue Cycle Management streamlines processes, maximizes reimbursements, and improves financial performance for healthcare providers. Medical Billing and Coding Hub Healthcare Solutions commits to providing superior billing administration, Medical billing Audit Services concentrating on nearly every facet of clinical or patient accounts. We work to ensure the most available timely compensation for our patients. "The quicker an invoice is ready, the swifter and more straightforward the payment is granted." We're working around the clock, and our billing experts are always available.

Q1. What Are Medical Billing Audit Services?
Up to
How Medical Billing Audits Improve Compliance
Medical billing audits play a crucial role in ensuring compliance with healthcare regulations by identifying errors, discrepancies, and potential fraud in billing processes. They help healthcare providers adhere to state and federal laws, including HIPAA and CMS guidelines, reducing the risk of penalties or legal issues. Regular audits promote accurate coding and billing practices, ensuring proper reimbursement from payers. Additionally, they enhance transparency and accountability in financial operations. By addressing compliance gaps, billing audits safeguard a provider's reputation and financial stability.
Medical billing audits play a crucial role in ensuring compliance with healthcare regulations by identifying errors, discrepancies, and potential fraud in billing processes. They help healthcare providers adhere to state and federal laws, including HIPAA and CMS guidelines, reducing the risk of penalties or legal issues. Regular audits promote accurate coding and billing practices, ensuring proper reimbursement from payers. Additionally, they enhance transparency and accountability in financial operations. By addressing compliance gaps, billing audits safeguard a provider's reputation and financial stability.

GET YOUR FREE REVENUE CYCLE MANAGEMENT ASSESSMENT
Evaluate your Practice Performance
We offers free revenue cycle assessments (RCAs) to help large and small practices to work smarter, not harder. Are you performing to your full potential?
Frequently Asked Questions

Medical billing audit services encompass a comprehensive examination of the billing and coding practices employed by healthcare providers to verify their accuracy, adherence to regulations, and appropriate reimbursement. Such audits are instrumental in detecting discrepancies, minimizing claim rejections, and enhancing the efficiency of the revenue cycle.
Billing audits assist healthcare providers in maintaining compliance, decreasing errors, and reducing the likelihood of claim denials. Additionally, they contribute to the accuracy of revenue, bolster financial performance, and protect against potential regulatory penalties.
Billing audits employ various tools such as coding software, electronic health record (EHR) systems, and data analytics platforms. The methodologies applied encompass claim sampling, trend analysis, and compliance checklists to verify accuracy and ensure conformity with regulations.
Medical billing audits find mistakes like wrong codes, wrong claims sent, and not getting paid correctly that can cause money to leak out. By rigorously examining accounts receivable and insurance remuneration, audits detect unreported fees, lost billing chances, or rejected billing instances that can be contested.
The frequency of medical billing audits depends on the size and intricacy of the clinic, along with the diversity of insurance providers and governance atmosphere. Nonetheless, it generally seems wise to carry out checks at least every 3 months or twice a year. Potentially hazardous activities, such as methods involving regular programming updates or novice employees, might advantage from increased scrutiny to maintain adherence and precision. Routine checks also ready procedures for outside checks and decrease the danger of fines.
