Proper dental billing is crucial in order to receive payment for the full value of the services provided, which is essential for the financial stability and success of a dental practice. Dental billing is a procedure that collects payment for dental services performed in your dental practice

Why is dental billing important?
The role of dental billing is significant for various reasons.
- It ensures the payment of dental practices which is critical to their financial stability and profitability.
- Accurate billing enables to maintain patient and insurance company trust.
- Accurate dental billing can minimize the risk of insurance company audits and financial penalties
Dental billing is important for several reasons:
- Reimbursement:
Dental insurance billing is necessary in order to receive reimbursement for the services provided to patients. Proper billing is crucial in order to receive payment for the full value of the services provided, which is essential for the financial stability and success of a dental practice.
- Compliance: Accurate and compliant insurance billing is important in order to avoid denied claims, audits, and legal action. Dental practices must understand and comply with the rules and regulations of the insurance companies they work with, as well as federal and state laws and regulations related to healthcare billing.
- Record Keeping: Billing is an important component of a practice’s record-keeping system. Accurate and complete records of billing and payment activities help practices monitor their financial performance and ensure that they receive payment for all services provided.
- Patient Satisfaction: Dental billing is also important for patient satisfaction. Patients want to know that their insurance coverage is being utilized to its fullest and that their out-of-pocket costs are being accurately calculated. Accurate and transparent billing helps to build trust between a practice and its patients.
7 Steps of Dental Billing
Following are various steps typically involved in the Dental Billing
- Pre-authorization
- Documentation for data collection
- Coding
- Claims preparation/Submission
- Account follow-up
- Payment posting
- Account management for receiving
- Pre-authorization: Obtaining pre-authorization from insurance companies or government programs for certain procedures.
- Documentation for data collection: Accurately documenting the services provided, including patient information, diagnosis codes, and procedures performed.
- Coding: Assigning the appropriate codes to the services provided using the Current Dental Terminology (CDT) codes.
- Claims preparation: Preparing and submitting claims to insurance companies, government programs, or patients. This may involve entering claims into an electronic billing system, printing and mailing paper claims, or submitting claims through an online portal.
- Account Follow-up: Following up on the status of claims to ensure payment is received. This may involve checking for payment status in an electronic billing system, calling insurance companies or government programs to inquire about the status of a claim, or appealing denied claims.
- Payment posting: Recording payments received from insurance companies, government programs, or patients. This may involve updating an electronic billing system, recording payments in a ledger, or depositing checks.
- Accounts Receivable Management: Monitoring accounts receivable and pursuing payment from insurance companies, government programs, or patients as needed.
Dental insurance and its types:
Dental insurance enables people and families pay for dental procedures and treatments.
Following are various types of dental insurance with its feature and benefits:
- Preferred provider organization plans (PPO)
- Plans offered be dental Health Organizations (DHMOS)
- Indemnity plans
- Discount dental plans
- Preferred Provider Organization plans:
PPOs are more flexible than DHMOS, covered broader range of procedures, including major dental work like crowns, bridges, and implants. Individual with PPOs can see any licensed dentist, but they may receive better benefits if they choose a provider from the plan’s network.
- Plans offered by Dental Health Maintenance Organizations:
These plans cover a limited number of preventive and primary dentist procedures such as cleanings, X-rays, and fillings. It typically requisite of individuals to select a primary dentist from network of providers and consequently minimize the coverage for operations performance by providers outside the network.
- Indemnity plans:
These plans provide the most flexibility in terms of selecting a dentist and the procedures covered. It enables the individuals to see any licensed dentist and receive benefits for various procedures.
- Discount Dental Plans:
Discounts dental plans provide members with discounts on dental procedures and treatments. Individuals join the plan for a fee and receive discounts on dental services performed by participating providers.
Common insurance terms for dental insurance coverage and billing:
Individual must be intimate with several common insurance terms to comprehend their dental insurance coverage and billing.
- Deductible:
The amount paid out of pocket by an individual before their insurance coverage kicks in.
- Coinsurance:
The individual is responsible for paying a portion of amount of the cost of a dental procedure after meeting the deductible.
- Co-payment:
An individual pays a set amount of money for a dental procedure, regardless of its cost.
- Maximum benefits:
The most money the insurance company will pay for dental procedures in a given year
- Pre-existing conditions:
Dental conditions or treatments that existed prior to enrollment in the insurance policy. The policy may not cover these conditions.
- Waiting period:
A stated period of time that a person must be enrolled in an insurance benefit plan before being eligible for benefits or for a specific category of benefits.
- Coordination of Benefits (COB):
A process that insurance carriers use to determine the order of payment and amount each insurance carrier will pay when a person receives dental services that are covered by more than one insurance benefit plan
What are some best practices for dental billing?
Following are best practices for dental billing:
- Staying up-to-date with time and insurance policies
- Using specialized software and billing service
- Maintaining of accurate records
- Stay up-to-date on changes in regulations and insurance policies: Dental billing industry and its rules sand regulations are changing rapidly. Consequently, it’s essential to stay informed and up-to-date. This can be possible by updating skills, education courses, reading industry publications or consulting specialists
- Use specialized software or a billing service:
To streamline the Billing procedure, it’s necessary to use specialized software to minimize the risk of errors. It also automate many routine tasks in billing process.
- Maintaining accurate and through records: Accuracy and complete documentation is key to the success of dental billing.
This includes
- Keeping up-to-date patient information,
- Documenting all services provided, and
- Following up on the status of claims in a timely manner.
Having a robust system for maintaining data enables to ensure the efficiency and smoothness of claims processed. It also reduces the claim denials and other issues as well.
What is illegal dental billing?
According to American Dental Association Dental insurance fraud is “any crime where an individual receives insurance money for filing a false claim, inflating a claim or billing for service not rendered”
Common fraudulent practices:
There are various billing claims habits that are fraudulent. The most common types of billing fraud are as following:
- Billing for incomplete and unperformed services
- Altering date of service
- Waiving deductibles
- Submitting a claim for treatment using a different member’s information
- Inappropriate usage of additional codes
Fraud harms everyone in the dental industry. It not only drives up the cost of coverage for patients and employers, but it can also directly affect your practice. Being found guilty of perpetrating fraud can result in fines, loss of network participation and professional licenses and even jail time.
Outsource your Dental Billing Services !
Outsource your dental billing to US Global Medical billing services and remove your administrative burden and work frustration.
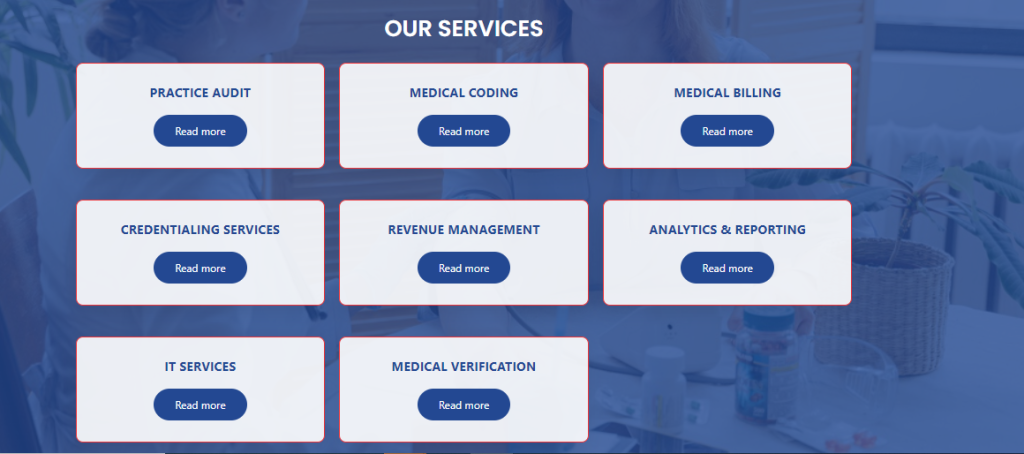
Medical B&C Hub Services Offer Services :
1. Dental Audit of Practice
2. Dental Medical Coding & Billing ( CPS,CCS Certified coder services )
3. Expert Credentialing Services.
4. Free Credentialing & EDI services.
Please visit our website:usglobalbs.com and get free consultation for 30 days Audit services.
Lets talk